Machine learning has recently entered the world of medical imaging and clearly offers the potential to revolutionize modern imaging. It refers to any algorithm that draws conclusions from data and learns and improves automatically when fed with more training data.
In radiology, data are mostly images and machine-learning algorithms are often colloquially referred to as “artificial intelligence” (AI). Prominent people have speculated that training of radiologists should be stopped, as machine learning is going to replace radiologists until 2021 (Read more on: Why Ai will not replace radiologists.). Well, 2021 has come and radiologists are still around and evaluating their patient’s images. Naturally, radiologists consider themselves as indispensable and this view is shared by many others, too. “Artificial intelligence” will most likely complement human intelligence and AI clearly offers the potential to make radiologists more efficient, improve the diagnostic quality - by standardizing workflow and guiding radiologists to potential findings - and to uncover hitherto unknown relations by mining from “big data”.
Thus, our research focuses on how machine learning algorithms can be brought into clinical practice and how they can support clinicians, both radiologist (if they are still around) and others.
Deriving Patients Diagnoses from Images:
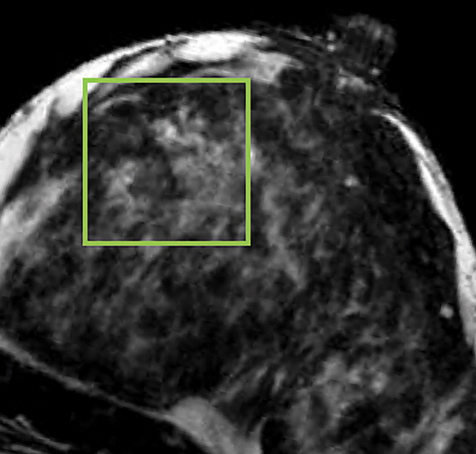
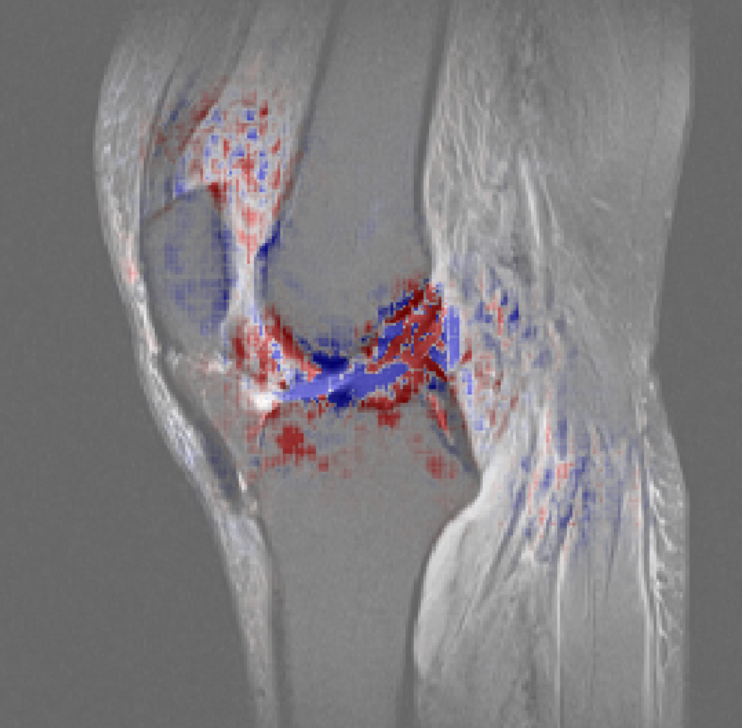
Machine-learning algorithms can be trained on specific questions such as: “Is there a tear of the cruciate ligaments?” or “Is there a malignant breast lesion in the MRI?”. University hospitals such as ours acquire vast amounts of images and reports describing the diagnoses are written by experienced radiologists all the time. We build upon this database to develop our algorithms.

Using Machine Learning to Generate New Tools:
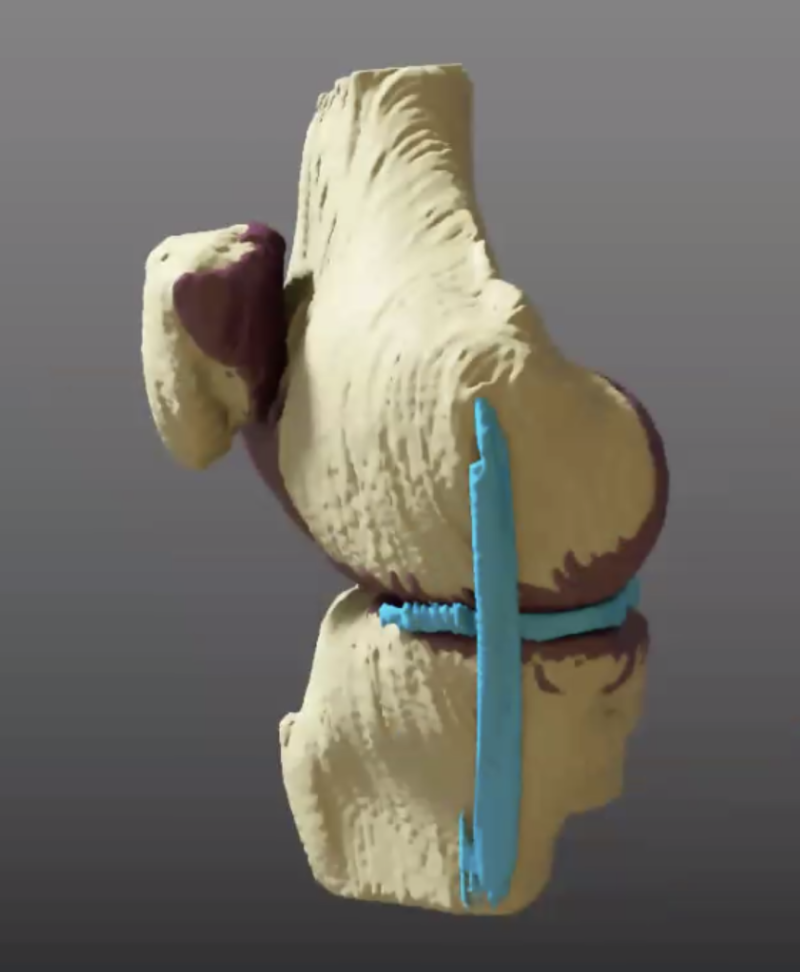
Image interpretation is intrinsically limited by what the human mind perceives. The human mind is well adapted to intuitive pattern recognition, less so to quantitative analyses. We use machine learning to generate and present data that is usually not accessible to radiologists such as quantitative measures of the relative positions of anatomic structures to each other (e.g. bones), average thickness, volume, and surface area (e.g. of articular cartilage), and texture patterns across 2D images or 3D volumes.

Advance Machine Learning Methodically:
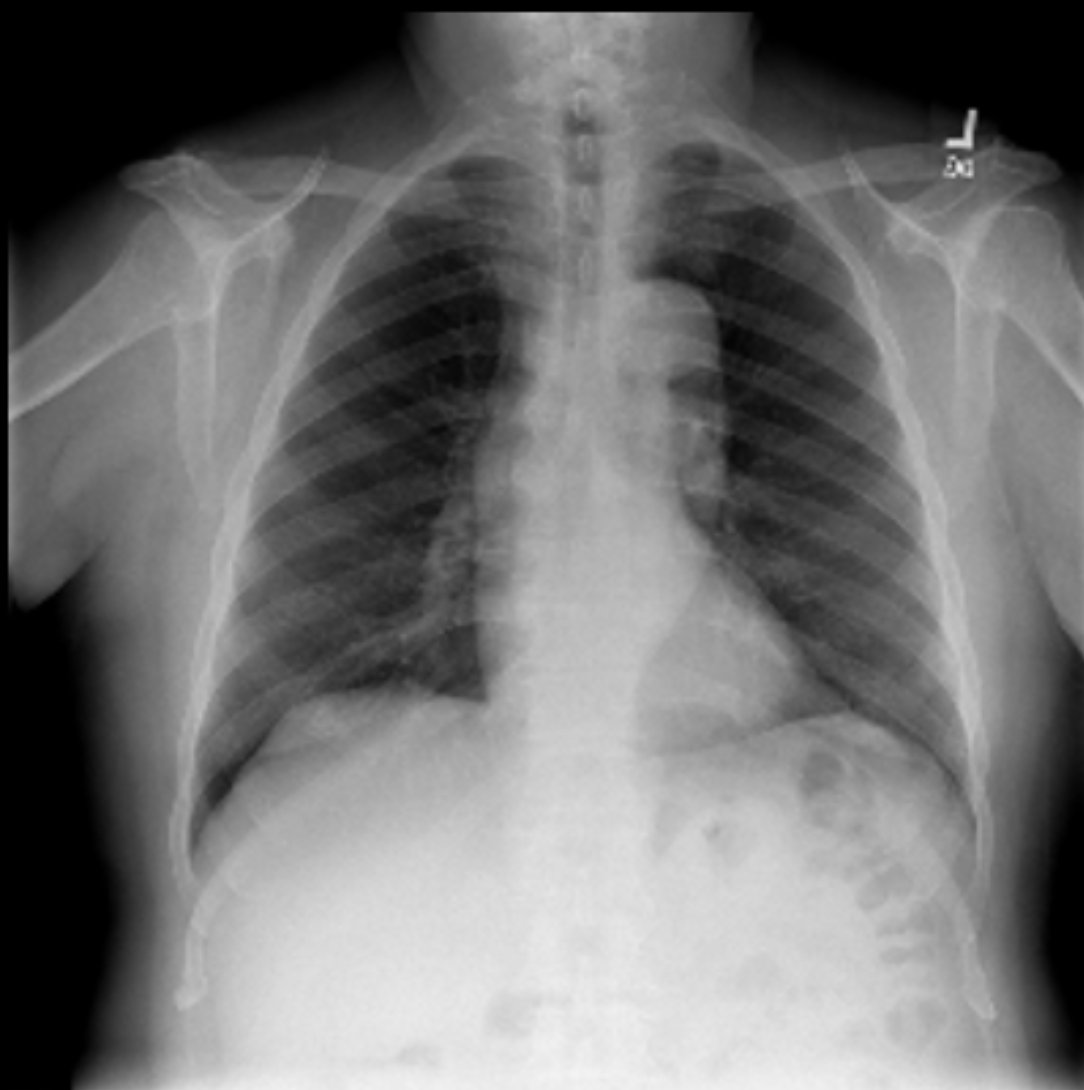
Machine learning in medicine requires vast amounts of data. The problem is that medical images are highly sensitive and cannot be shared easily to create even larger databases. We work on creating “artificial” radiological images that can be shared without disclosing patient-specific and sensitive information or that can also be used to generate new tools for teaching clinicians on how to interpret radiological images.

What is our goal ?
We want to advance machine learning algorithms so that they can bring real clinical benefit to the clinician, the patient, and the entire health infrastructure. To this end, we collaborate closely with fellow clinical radiologists, other clinical disciplines, imaging and big data scientists as well as others.
Funding is provided both internally (by the Departments of Diagnostic and Interventional Radiology in Aachen and Düsseldorf) and externally by national funding agencies (e.g. DFG).